--most common cause of intestinal obstruction in kids 3 months-6 years of age.
--male:female ratio is 4:1
--Seasonal variation with peaks after GI viral illness seasons.
PATHOPHYSIOLOGY
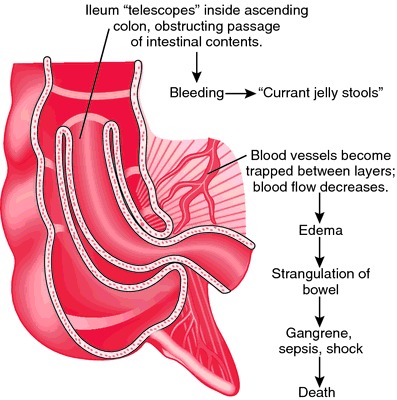
--In younger children, the ileum invaginates into the upper colon, bringing the mesentery with it (ileocolic).
PATHOPHYSIOLOGY
--In younger children, the ileum invaginates into the upper colon, bringing the mesentery with it (ileocolic).
--lead point is often lymphoid hyperplasia from viral gastroenteritis.
--In older children, ileo-ileo intussusceptions are more common.
--lead point causes include intestinal polyps, Meckel diverticulum, lymphosarcoma, or even HSP
--Constriction of the mesentery obstructs venous return, leading to bowel ischemia and bloody stools leading to the classic “currant jelly” stool, which is a late finding occurring in about 50% of cases.
CLINICAL FEATURES
CLINICAL FEATURES
--Sudden colicky abdominal pain (child will stop, cry, draw up their legs, and then after a few minutes the child appears well).
 --As the condition progresses the time between episodes decreases.
--As the condition progresses the time between episodes decreases. --Stool is generally guaiac positive even in the absence of gross blood.
--A palpable sausage shaped mass can be found on the right side of the abdomen in about 2/3 of cases
DIAGNOSIS
--Diagnosis often made by history alone
--KUB may suggest a filling defect in the right lower quadrant of the abdomen or can be normal
--US can often show the classic target appearance of bowel within bowel (donut sign (transverse); sandwich sign (longitudinal)
TREATMENT
--Air contrast enema is preferred over barium enema because it enables better control over colonic pressure and in the case of perforation prevents barium spillage into the peritoneum.
--Children generally admitted for observation because of the 5-10% recurrence rate. A second attempt at air reduction is usually successful, but if further recurrences occur surgical reduction may be necessary.
--Air contrast enema is preferred over barium enema because it enables better control over colonic pressure and in the case of perforation prevents barium spillage into the peritoneum.
--Children generally admitted for observation because of the 5-10% recurrence rate. A second attempt at air reduction is usually successful, but if further recurrences occur surgical reduction may be necessary.
10-SECOND RECAP:
--most common in kids 3 mo-6 yrs old; male:female 4:1
--ileocolic (younger), ileo-ileo (older), or wherever--common lead points (lympoid hyperplasia from gastroenteritis, polyps, meckel's, cancer, HSP, etc.)
--bowel ischemia -> guaiac+ stool -> occasionally currant jelly stool
--history is key, palpable sausage in RLQ in 2/3, KUB maybe, ultrasound (donut/sandwich signs)
--air contrast enema = diagnostic + therapeutic; surgery if that doesn't work
Submitted by J. Grover.


No comments:
Post a Comment