--lots of overlap in signs/symptoms
--one article came up with a decent decision rule
J Bone Joint Surg Am. 1999 Dec;81(12):1662-70.
--looked at 282 cases, excluded 114 atypical patients (e.g. immunocompromised), leaving 168
--38 had "true" septic arthritis
--septic arthritis defined by positive culture or joint WBC >= 50,000 cells/mm3
--four things they decided on that might differentiate:
- history of fever
- non-weight-bearing
- erythrocyte sedimentation rate (ESR) >= 40 mm/hr
- serum WBC > 12,000 cells/mm3
--predicted probability of septic arthritis using these four predictors:
- < 0.2 percent for zero predictors
- 3.0 percent for one predictor
- 40.0 percent for two predictors
- 93.1 percent for three predictors
- 99.6 percent for four predictors
BOTTOM LINE:
--septic arthritis is bad, transient synovitis not so bad
--hard to tell sometimes, signs/symptoms are often similar
--useful: history of fever, non-weight bearing, ESR>40, WBC>12k
--if none of the above: unlikely septic arthritis
--more of the above: worry a bit more
Submitted by S. Lee.
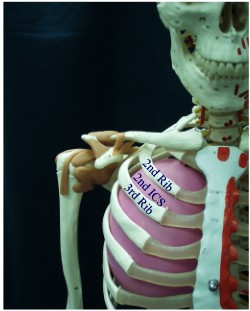
Reference(s): kocher article, picture